The Ministry of Health has made a huge naloxone mis-step. But it’s not too late to fix it.
Attention all Ontarians: Prepare for a spike in opioid poisoning deaths.
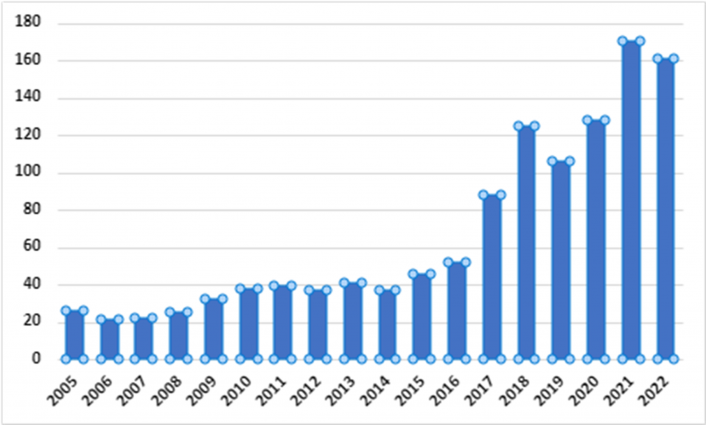
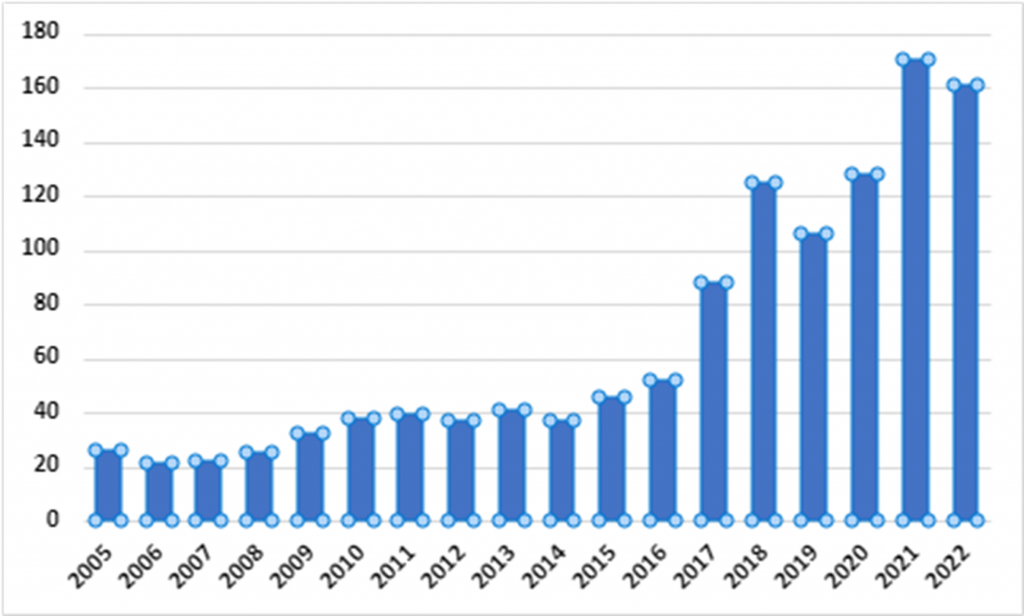
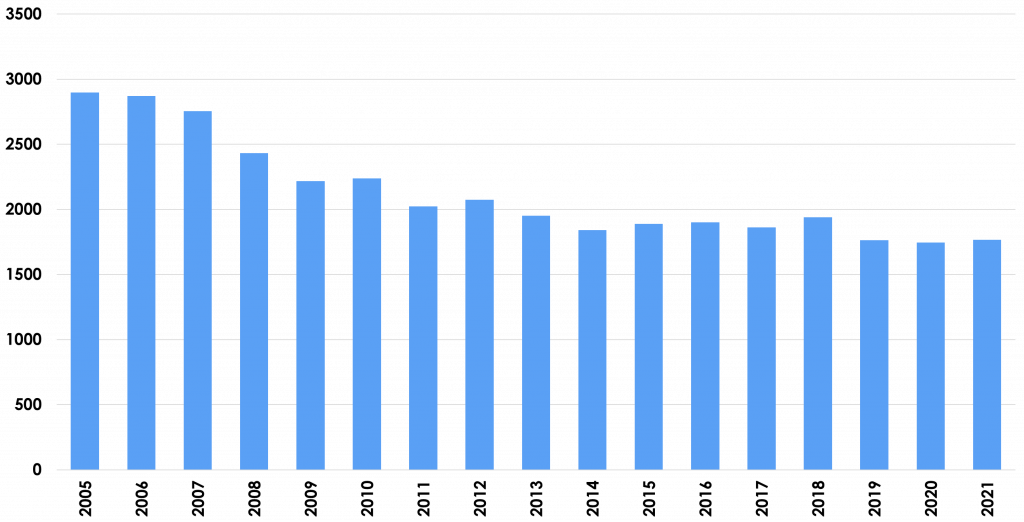
As a licensed pharmacist of 30 years practicing in Hamilton, I have watched the opioid crisis emerge and take the lives of friends and loved ones, including my dear late friend, Rebecca Morris-Miller. Between January 2016 and June 2023, there were an estimated 40,000+ opioid toxicity deaths in Canada, outnumbering motor vehicle fatalities by 5x in 2021, which have, thankfully, been slowly, but steadily declining due to the efforts and resources expended towards that effort. We need to do the same for the opioid crisis, but recent changes announced by the Ministry of Health are a massive step backwards, and are sure to result in more lives lost.
Our pharmacy team has dedicated itself to fighting the opioid crisis through supporting the Four Pillars approach adopted by the City of Hamilton Drug Strategy, for which I was the pharmacist representative. We collaborate with scores of community-based organizations (CBOs) and passionate people across the city in our mission of hope. It goes without saying that one of the main objectives of the Strategy is achieve a turnaround to the crisis as fast as humanly possible.
Since 2016, Ontario pharmacists have been funded by the Ministry of Health to offer naloxone kits and training through the Ontario Naloxone Program for Pharmacies (ONPP) to individuals and community-based organizations (CBOs) that serve individuals at risk. Those CBOs that were not linked to a pharmacist could access kits through Public Health via the Ontario Naloxone Program (ONP) – click here to see a copy of the previous policy FAQs.
On February 9th, 2024 the Executive Officer of the Drug Programs Branch at the Ontario Ministry of Health announced sweeping changes to the pharmacy program (ONPP). The changes announced will only serve to raise barriers to accessing life-saving naloxone, and contribute directly to the death of untold numbers of people at risk. – click here to see a copy of the announced changes.
(Before we go any further, let’s get two things straight: First, the single biggest employment group that is affected by opioid poisoning deaths is the construction sector (one-third). These are hard-working, dedicated people (mostly men) simply trying to provide for their families. They often engage in injurious and precarious work, and risk not being permitted to work if they report an injury to their foreman. As a result, they will often ask their co-workers to share their pain medications, and this often leads to problems. We cannot remain silent while some try to demonize and mischaracterize the people that keep our lights on and our cars on the roads. They, like all people, deserve respect, dignity, and our support. Second, anyone can experience an accidental opioid poisoning. Anywhere opioids exist, there is a potential risk. Naloxone training is not just for opioid users or former users, or their family members. It is simply an extension of first aid training, which any person willing to save someone else’s life should be able to access.)
The changes prohibit, with immediate effect, all of the following for ONPP pharmacies:
- Providing naloxone kits to businesses and/or organizations
- Providing naloxone kits off-site from the physical premises of the pharmacy
- Providing training other than on an individual basis (which seems to be the same as…)
- Providing training in group settings
- Providing training other than in-person
For the record, we have never provided kits to businesses. Every kit we have provided was to individuals for their own personal possession. Every person has either been trained by us, or has had their previous training affirmed. The really massive impact of Sweeping Change #1 is that all of the CBOs that rely on us for timely, reliable access to kits for their clients are now immediately cut off from further supply. I suppose they will be expected to source through the Ontario Naloxone Program (ONP, i.e. Public Health), for whom I have great respect as a mission partner. However, the ONP is infinitely less accessible or reliable than pharmacies for naloxone supply, and pharmacists are the most obvious professionals to provide the highest quality training possible. New ONP agreements routinely take 2 months to execute, and that was before the recent wave of cuts to Public Health. Our CBO partners are left utterly bereft, and are absolutely incensed by this change. Count on hearing from them very soon.
Sweeping Change #2 means that the outreach work that pharmacists are doing in shelters, churches, colleges and universities, at music venues, at City Halls, at outdoor fairs, even in high schools (where I believe it is needed more than anywhere) – all places where people need to hear about the risks associated with opioids, that there is help available if they are going through difficulties, that if they are going to use drugs, not to use alone and instead call the National Overdose Response Service (NORS.ca), and how they might save someone else’s life using naloxone, are all now cast aside.
Change #2 also means that all persons must now physically come to the pharmacy, every single time they need kits, even if they have already been trained and just need replacement kits (with some exceptions). This unfairly discriminates against:
- unhoused persons, (again, often former tradesmen, victims of domestic violence. “They” could easily be you or me.)
- people who already have regular prescription deliveries from their pharmacy, requiring them to make an unnecessary trip to get naloxone
- people whose local pharmacies don’t participate in the ONPP
- people living in remote areas, where the nearest pharmacy may be a very long drive. Indigenous communities across the province already struggle with access to naloxone kits.
Sweeping Changes #3 and #4 require that training “must be provided on an individual basis,” and “not in group settings”. Under the new rules, if a couple comes into the pharmacy for naloxone training, I now have to tell one of them to wait 15 minutes until their partner is trained first? Really? Is this a step towards “as fast as humanly possible”, or 20 steps back? The Ministry needs to find ways to facilitate, not discourage, group training. Recently, the Michael G. DeGroote School of Medicine at McMaster University reached out to me to provide our renowned 2-hour opioid crisis/naloxone training to its undergraduate students (Ontario’s future doctors) – a landmark achievement for us. This validated the reputation of our training program as being of the highest quality and value. This is now dead in the water.
Sweeping Change #5 may be the most shocking of all. It is incomprehensible that, in the 21st century when health professionals (including pharmacists) are providing, and the public is demanding, the use of virtual tools to deliver healthcare services, that individuals will now be forced to go to a pharmacy to get their training and kits. This means, for example, that training can no longer be delivered via Zoom, which was the only means we had during the pandemic, and saved countless lives. Prohibiting it defies all sense and logic.
Therefore, it is with the utmost sense of urgency that I implore Minister of Health and Deputy Premier Hon. Sylvia Jones, out of compassion and humanity, to immediately reverse this policy decision and not to undertake any further changes without consulting with our partner agencies and the people that will be most affected, including: Grenfell Ministries, NORS, YWCA, Mission Services Hamilton, Shelter Health Network, Hamilton Social Medicine Response Team, The AIDS Network, De dwa da dehs nye>s Aboriginal Health Centre, The Chiefs of Ontario, Fort Albany First Nation, Eabametoong First Nation (Fort Hope), The Good Shepherd, The Hamilton Hub, The Greater Hamilton Health Network, Compass Community Health, Mohawk College, trios College, and McMaster University, to name but a few. Let’s collaborate on ways forward that don’t put Ontarians’ lives at risk. It is literally a matter of life and death.
Hamilton, Ontario Opioid-related Deaths. Source: https://www.hamilton.ca/people-programs/public-health/alcohol-drugs-gambling/hamilton-opioid-information-system#deaths
Motor Vehicle Fatalities, Canada. Source: https://tc.canada.ca/en/road-transportation/statistics-data/canadian-motor-vehicle-traffic-collision-statistics-2020
NEVER USE ALONE! Call NORS or visit www.nors.ca